By Dr. Mercola
While many health screens and lab tests are overrated or unnecessary, there are a few that are vitally important, such as vitamin D. I recommend checking your vitamin D level at least twice a year.
Two other really important tests are serum ferritin (which measures stored iron) and gamma-glutamyl transpeptidase or sometimes called gamma-glutamyltransferase (GGT; a liver enzyme correlated with iron toxicity, disease risk and all-cause mortality). By monitoring your serum ferritin and GGT levels and taking steps to lower them if they’re too high, you can avoid serious health problems.
For adults, I strongly recommend getting a serum ferritin test and GGT on an annual basis. When it comes to iron overload, I believe it can be every bit as dangerous to your health as vitamin D deficiency. In this interview, Gerry Koenig,1 former chairman of the Iron Disorders Institute and the Hemochromatosis Foundation, explains the value of these two tests.
Iron Overload Is More Common Than Iron Deficiency
Iron is one of the most common nutritional supplements. Not only can you get it as an isolated supplement, but it’s also added to most multivitamins. Many processed foods are also fortified with iron. While iron is necessary for biological function, when you get too much, it can do tremendous harm.
Instant Access to Current Spot Prices & Interactive Charts
Unfortunately, the first thing people think about when they hear “iron” is anemia, or iron deficiency, not realizing that iron overload is actually a more common problem, and far more dangerous. Many doctors don’t understand or appreciate the importance of checking for iron overload.
Virtually all adult men and postmenopausal women are at risk for iron overload due to inefficient iron excretion, since they do not lose blood on a regular basis. Blood loss is the primary way to lower excess iron, as the body has no active excretion mechanisms. Another common cause of excess iron is the regular consumption of alcohol, which will increase the absorption of any iron in your diet.
For instance, if you drink wine with your steak, you will likely absorb more iron than you need. There’s also an inherited disease, hemochromatosis, which causes your body to accumulate excessive and dangerously damaging levels of iron.
If left untreated, high iron can contribute to cancer, heart disease, diabetes, neurodegenerative diseases and many other health problems, including gouty arthritis. In one small study,2 100 percent of the patients achieved marked reduction in attacks or complete remission after phlebotomy was used to remove iron and maintain an iron level at near-iron deficiency — “the lowest body iron store compatible with normal erythropoiesis and therefore absence of anemia.”
Iron causes all this harm by catalyzing a reaction within the inner mitochondrial membrane. When iron reacts with hydrogen peroxide, hydroxyl free radicals are formed. These are among the most damaging free radicals known, causing severe mitochondrial dysfunction, which in turn is at the heart of most chronic degenerative diseases.
GGT Is a Potent Predictor of Mortality
GGT is a liver enzyme involved in glutathione metabolism and the transport of amino acids and peptides. Not only will the GGT test tell you if you have liver damage, it can also be used as a screening marker for excess free iron and is a great indicator of your sudden cardiac death risk.
In recent years, scientists have discovered GGT is highly interactive with iron, and when both your serum ferritin and GGT are high, you are at significantly increased risk of chronic health problems, because then you have a combination of free iron, which is highly toxic, and iron storage to keep that toxicity going.3
“Recently, [GGT] was proven by the life insurance industry as the single measure that is most predictive of early mortality,”4,5Koenig says. “In other epidemiological studies, it’s linked to pretty much every cause of death,6 because it provides those free radicals and hydroxyl radicals …
I believe that … people born after World War II are now at greater risk because of the environmental toxicants we face … Basically, reduction in glutathione levels — your body’s most important antioxidant — is indicated by an increase in GGT …
[G]lyphosate, excess iron, all of the substances in the environment — whether you take it in as food or it’s in the air — that utilize your body’s toxic waste disposal system in some way [will] reduce your antioxidants, whether it’s vitamin D, cholesterol, vitamin E or vitamin A. A reduction of those makes you more vulnerable to disease, particularly chronic disease and autoimmune diseases across the board.”
Ideal GGT and Iron Levels
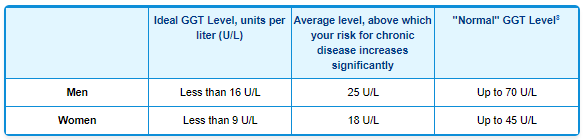
As with many other lab tests, the “normal” ranges for GGT and serum ferritin are far from ideal.7 If you’re in the “normal” range, you’re virtually guaranteed to develop some sort of health problem. Based on Gerry’s recommendation I had my GGT tested last month and it was 17, which is healthy especially since my ferritin level is 37. You really need both tests to confirm lack of iron toxicity as he explains in the full interview.
According to Koenig, women with a GGT above 30 U/L have a higher risk of cancer and autoimmune disease. Interestingly, while for most other tests the range between what’s healthy and what’s risky tends to be quite broad, in the case of GGT, the range between health and disease is in the single digits.
“Part of it is dependent on body weight,” Koenig says. “Strangely enough, the most recent indications are that people who are too thin (whatever their level of GGT is), it could be harmful if [their GGT is] relatively high.9 For instance, for a thin woman with a GGT … in the range of the second quartile, which is going to be generally 14 to 18 today it can be dangerous if she’s expecting to have children and has a very low BMI.”10
When it comes to serum ferritin, a level of 200 to 300 nanograms per milliliter (ng/mL) falls within the normal range for women and men respectively, which is FAR too high for optimal health. An ideal level for adult men and non-menstruating women is somewhere between 30 and 60 ng/mL.
You do not want to be below 20 ng/mL or above 80 ng/mL. The most commonly used threshold for iron deficiency in clinical studies is 12 to 15 ng/mL.11 Maintaining a healthy iron level is also important during pregnancy. Having a level of 60 or 70 ng/mL is associated with greater odds of poor pregnancy outcomes.12 That said, iron deficiency during pregnancy is equally problematic, so make sure you get tested.
Last but not least, since the ferritin and GGT are interactive, low GGT tends to be protective against higher ferritin. So, if your GGT is low, you’re largely protected even if your ferritin is a bit higher than ideal. Still, it would be wise to take steps to lower your ferritin to a more ideal level nonetheless. On the other hand, even if your ferritin is low, having an elevated GGT levels is cause for concern, and needs to be addressed.
When Might a Transferrin Saturation Test Be Useful?
If you are thin, with a body mass index (BMI) below 22 or 23, Koenig suggests getting a transferrin test as well, which gives you a percentage saturation level. A level of 25 to 35 percent is typically considered healthy. In the 1970s, the transferrin saturation test was used as a marker for early death. Having a transferrin saturation percentage of over 55 indicated a 60 percent increased risk for premature death.
At that time, an estimated 2.6 percent of the U.S. population had transferrin saturation percentages that high. Today, it’s down to half of that, in large part because of the increase in obesity, which “dilutes” your saturation percentage, and the transferrin test is no longer used as a marker for early death. However, if you are very thin, it can still be a useful test.
“Anything between 25 and 35 is safe. If you’re unusually thin, I would get that test because there you could have unsuspectingly high transferrin saturation, particularly if you’re malnourished … Anorexia nervosa has severe effects on the brain when you’re that thin and your BMI is at 14 or 15,” Koenig says.
Why Excess Iron Is so Dangerous
Your body creates energy by passing the electrons from carbs and fats you eat as fuel to oxygen through the electron transport chain in your mitochondria to produce adenosine triphosphate (ATP). Ninety-five percent of the time, the oxygen is converted to water. But 0.5 to 5 percent of the time, reactive oxygen species (ROS) are created. ROS are not all bad as they are important biological signaling molecules, but excessive ROS leads to mitochondrial damage and dysfunction.
Iron can react with hydrogen peroxide in the inner mitochondrial membrane. This is a normal part of cellular aerobic respiration. But when you have excessive iron, it catalyzes the formation of excessive hydroxyl free radicals from the peroxide, which decimate your mitochondrial DNA, mitochondrial electron transport proteins and cellular membranes. This is how iron overload accelerates chronic disease.
If you eat excessive net carbs (total carbs minus fiber) the situation is further exacerbated, as burning carbs as your primary fuel can add another 30 to 40 percent more ROS on top of the hydroxyl free radicals generated by the presence of high iron.
Unfortunately, most people reading this are burning carbs as their primary fuel. If you struggle with any kind of chronic health problem and have high iron and eat a standard American diet that is high in net carbs, normalizing your iron level (explained below) and implementing a ketogenic diet as described in my book, “Fat for Fuel,” can go a long way toward improving your health.
Taking extra antioxidants to suppress ROS generated by high iron alone or in combination with a high-sugar diet is inadvisable, as ROS also act as important signaling molecules. They’re not all bad. They cause harm only when produced in excess.
Your best bet is to lower the production of ROS. One of the easiest and most effective ways to do that is to eat a diet high in healthy fats, adequate in protein and low in net carbs. Eating healthy fats can make a bigger difference than you might think, especially if you have high iron.
How to Lower Your Iron
The good news is it’s easy to lower your iron level if it’s too high. One of the easiest ways is simply to donate blood two or three times a year. If you have severe overload you may need to do more regular phlebotomies. Two years ago, my ferritin was 150 ng/mL. I implemented self-phlebotomy where I would take out anywhere from 2 to 6 ounces of blood every few weeks, which brought me below 100 ng/mL.
I stopped the phlebotomy when I started a comprehensive detoxification strategy involving near and far infrared sauna, and interestingly, despite the fact I was no longer removing blood, my ferritin continued to drop over the next nine months. Now, it’s down to 37 — far lower than I was ever able to get down to with therapeutic phlebotomies, and as I mentioned earlier I have a healthy GGT level of 17.
As it turns out, an effective detoxification program can lower iron as well. While this was a surprise to me, Koenig confirms that this has indeed been documented by Dr. F.S. Facchini in some of his research on iron. While I’ve long recommended donating blood as the solution to iron overload, I now believe a balanced approach using phlebotomy, detoxification and reducing dietary iron, especially meat, is the best way to go about it.
Keep in mind that trying to control high iron through your diet alone can be risky, as you will also forgo many valuable nutrients. That said, to avoid maximizing iron absorption, avoid eating iron-rich foods in combination with vitamin C-rich foods or beverages, as the vitamin C will increase iron absorption. If needed, you could also take a curcumin supplement. Curcumin acts as a potent chelator of iron and can be a useful supplement if your iron is elevated.
How to Lower Your GGT
GGT is inversely related to glutathione, a potent antioxidant produced in your body. As your GGT level rises, your glutathione goes down. This is part of the equation explaining how elevated GGT harms your health. By elevating your glutathione level, you will therefore lower your GGT. The amino acid cysteine, found in whey protein, poultry and eggs, plays an important role in your body’s production of glutathione.
Red meat, which does not contain cysteine, will tend to raise GGT, as will alcohol, so both should be avoided.13 Research also suggests eating at least 10 servings of fruits and vegetables rich in in vitamin C, fiber, beta-carotene, anthocyanins and folate per week can help reduce GGT.14,15 Examples include carrots, romaine lettuce, spinach, sweet potatoes, apricots and tomatoes.
Also, be aware that certain medications can raise your GGT. If this is the case, please confer with your doctor to determine whether you might be able to stop the medication or switch to something else, and avoid over-the-counter medicines, including ibuprofen and aspirin, both of which can damage your liver.
General detoxification is another important component if your GGT is high, as your liver’s job is to remove toxins from your body. The fact that your GGT is elevated means your liver is under stress.
The Protein-Iron-GGT Connection
I personally typically eat only 2 to 4 ounces of meat per week Americans tend to overeat meat in general, and most of it is dangerous CAFO meat loaded with toxins. Additionally, while the meat supplies you with more iron than you likely need, excess protein can also cause problems. Another little-known fact is that giving iron to a person who is malnourished and cannot process protein properly can be extremely dangerous. Koenig explains:
“I’ve been studying malnutrition for several years now, mainly kwashiorkor (also known as protein-calorie malnutrition), which is a typical malnutrition disease, along with marasmus in developing countries. There you have a situation where the children, particularly in kwashiorkor, cannot synthesize important proteins because of essential amino acid deficiencies …
[When] giving iron too early in a recovering child with kwashiorkor, or an adult for that matter, the measure that skyrockets early on, in that particular case, happens to be GGT.
High amounts of free iron [are dangerous] because they don’t have the proteins to safely contain that iron into either transferrin, which is the protein that protects the body from the iron in the bloodstream, or ceruloplasmin, which is necessary for copper transport. To get iron safely into the brain, it needs to be complexed with ceruloplasmin. Those can’t be synthesized in a malnourished person. [So, giving] iron to a malnourished person is highly toxic.”
African and Chinese Research Confirm GGT’s Relation to Chronic Disease
Koenig recently found a few African studies showing the importance of GGT. In the 1990s, when GGT was tested broadly in the U.S. as part of the National Health and Nutrition Examination Survey III (NHANES III, 1988 to 1994), results revealed that African-Americans had higher levels of both serum ferritin and GGT than Caucasians and Hispanics.
“Back then, those measurements were compared to measurements in Zimbabwe. In [Zimbabweans] who were not exposed to spraying for mosquitoes … the [ferritin and GGT measurements] were roughly half.
They had obviously been on a native diet … But I found, through several papers recently submitted in South Africa, that those measurements now are very high. They’re catching up and probably surpassing the American Blacks’ measurements, and they’re suffering the [same] chronic diseases …”
More recent studies from South Africa depict increasing GGT levels are associated with insulin resistance and cardiometabolic disease risk.16 Moreover, a recent Chinese study showed that while having a GGT level above the midpoint raised the risk of chronic kidney disease, when combined with high serum ferritin, that risk increased nearly fivefold.17 Other common diseases associated with high iron and GGT include diabetes, heart disease and cancer.
Blood Donations Lead to Radical Reduction in Disease
A number of epidemiological studies have also documented a significant reduction in chronic diseases among those who donate blood two or three times a year — findings that support the notion that iron overload is prevalent, and contributes to chronic disease. In some, heart disease and cancer were reduced by as much as 50 percent, Koenig notes.
Unfortunately, many doctors are still unaware of the importance of checking for iron overload (based on ideal levels and not what’s considered normal), and may overlook the GGT test as well.
“One of the reasons it’s difficult to get doctors to order GGT tests is they’re discouraged because they know some prescription drugs increase [GGT]. Although the overall effect may be protective, it’s not a happy situation to see a measure of disease increase just by taking a drug. There’s resistance in that area of getting tested. But it’s a pretty simple test. It would be recommended. And blood donation basically keeps one healthy,” Koenig says.
In summary, if you’re concerned about maintaining your health and preventing chronic disease, I would strongly encourage you to get a ferritin and a GGT test regularly, and if needed, implement the strategies discussed above to get them into their optimal ranges.
Serum ferritin and GGT are markers for iron toxicity, which is a major mostly unrecognized contributor to heart disease, cancer, diabetes, nonalcoholic fatty liver disease and many other chronic diseases. High iron even increases your risk of infections. As noted by Koenig, you really don’t want to check into a hospital with high iron, as your risk of contracting a hospital-acquired infection will be that much greater. The good news is, it’s so easy to turn around, thereby dramatically reducing your risk.
More Information
To learn more, I recommend visiting HealtheIron.com, where you can also order your serum ferritin and GGT tests or either of their special FeGGT-LifePRO™ test panels. If either serum ferritin or GGT is elevated, you need to take action. The treatment couldn’t be simpler. Unless you’re a menstruating woman, simply donate blood two to three times a year. If you do not qualify to donate blood, ask your doctor to write you a prescription for therapeutic phlebotomy.
Sources and References
- 1 Hemochromatosis.org
- 2 Rheumatology 2003 Dec;42(12):1550-5
- 3 Disease Markers 2015; 2015: 818570
- 4 Leading Contributors to Mortality Risk in Life Insurance Applicants
- 5 Journal of Insurance Medicine 2012;43(3):162-8
- 6 Clinical Chemistry 2007; 53(5): 940-946
- 7, 8 Irondisorgers.org, Four Important Tests Where Ranges for Normal Vary (PDF)
- 9 Biomedical Reports March 2016; 4(3): 307-312
- 10 Diabetes Care. 2014;37(7):1878–1884
- 11 Transfusion Medicine April 20, 2017, DOI: 10.1111/tme.12408
- 12 Mercola.com, Gerry Koenig Interview, June 12, 2016
- 13 American Journal of Clinical Nutrition April 2004; 79(4): 600-605
- 14 European Journal of Clinical Nutrition (2008) 62, 60–67
- 15 Livestrong March 2, 2012
- 16 European Journal of Preventive Cardiology 2014 Dec;21(12):1541-8
- 17 Disease Markers 2017; 2017:9765259